As a pediatric physical or occupational therapist, you’re likely aware that pelvic floor dysfunction affects children, not just adults. Yet, despite recognizing its prevalence, many therapists don’t feel equipped with the tools, training, or time to address bowel and bladder issues effectively. Unfortunately, this knowledge gap can leave children struggling with symptoms like bedwetting, fecal incontinence, or constipation for far too long.
If you’re a general pediatric therapist with young patients showing these issues, do you hesitate to treat them due to a lack of knowledge or confidence? Are these myths reinforcing any limiting beliefs you might have?
In this blog, we’ll address 5 myths surrounding pediatric pelvic floor dysfunction and why it’s essential for pediatric PTs and OTs to understand and address these issues. As a therapist, you’re in a prime position to make a difference in the lives of these children by expanding your knowledge and adding pelvic floor therapy to your skillset. Don’t let uncertainty prevent you from delivering effective treatments to the children and families who need your support the most.
Myth #1: Children Can’t Have Pelvic Floor Dysfunction
One of the most common misconceptions among laymen is that pelvic floor dysfunction only affects adults. Pelvic floor muscles are typically associated with childbirth and aging. However, children can experience pelvic floor dysfunction, and it’s more common than many realize.
This misconception can lead to a lack of awareness among parents about the prevalence of pelvic floor dysfunction in children.
Fact: Children are not small adults! So although children’s pelvic floor anatomy is different as they grow and develop, kids can have pelvic floor dysfunction too. These pediatric issues can go unnoticed or unaddressed during childhood, leading to complications in adulthood.
Pelvic floor muscles in children can become dysfunctional due to impaired growth and development during infancy and childhood, poor muscle coordination, or habitual holding patterns. This dysfunction can manifest as difficulty with urination or bowel movements, bedwetting, or urinary frequency. Left untreated, these problems can persist and worsen over time, impacting the child’s development and well-being.
As a pediatric therapist, you likely encounter children with these symptoms regularly, even if they’re not diagnosed with pelvic floor dysfunction. By recognizing the role the pelvic floor plays, you can be instrumental in helping these kids. My Peds Level 1 course covers the basics of pediatric pelvic anatomy and how to detect dysfunction early.

Myth #2: Children Will Outgrow Pelvic Floor Issues
A common misconception among healthcare providers and parents is that children will naturally “grow out” of pelvic floor issues, leading to a “wait-and-see” approach.
Fact: While time can sometimes resolve mild cases, this mindset can delay proper intervention and treatment. Untreated pelvic floor dysfunction can lead to long-term issues, including chronic constipation, urinary incontinence, and social-emotional challenges like anxiety or low self-esteem. Early intervention can prevent these problems from escalating.
As a pediatric therapist, you know the value of early intervention. Addressing pelvic floor dysfunction early can dramatically improve a child’s quality of life. In my Peds Level 1 course, I provide you with strategies for recognizing these issues and offering therapeutic solutions before they become long-term problems.
Myth #3: Pelvic Floor Therapy Is Only For Girls
Pelvic floor therapy is often mistakenly seen as something primarily for women and girls, due to its association with women’s health issues. This leads many parents and healthcare providers to overlook pelvic floor issues in boys.
Fact: Both boys and girls can experience pelvic floor dysfunction. Anatomical malformations, such as hypospadias or syringocele can lead to different urinary conditions in boys, just as conditions like vaginal reflux or labial adhesions can impact girls.

However, it’s important to remember that growth and development affect the pelvic floor in both sexes. Pelvic floor dysfunction can arise not only from these anatomical differences but also from impaired muscular strength and coordination, postural deviations, and behavioral patterns—issues common to both boys and girls. These problems can have a significant impact on their social life and self-esteem if left untreated.
With the right training, you can help these children develop proper pelvic floor function early, setting them up for long-term health and success. My Peds Level 1 course covers treatment protocols for both boys and girls, ensuring that you feel confident treating all your pediatric patients.
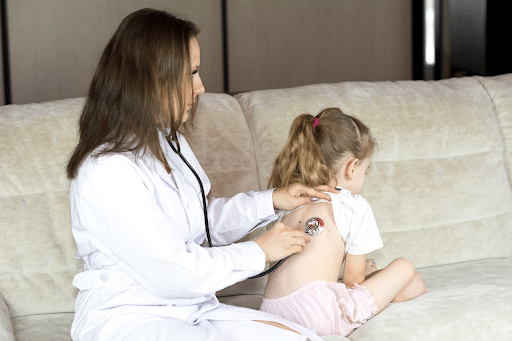
Myth #4: Pediatric Pelvic Floor Dysfunction Is Only Treated By Urology or Gastroenterology
Pediatric therapists may believe that pelvic floor dysfunction is strictly a “medical doctor’s” issue and should be handled by urologists or gastroenterologists, rather than addressed by physical or occupational therapists.
Fact: While bowel and bladder issues can involve the urinary and digestive systems, it’s often a musculoskeletal or behavioral issue that pediatric therapists are well-suited to treat. Problems like constipation, improper toileting postures, or overactive pelvic muscles fall directly within the scope of pediatric PT and OT. By addressing these underlying causes through exercises, biofeedback, and behavioral strategies, you can provide holistic care that reduces symptoms and improves quality of life.
Still, appropriate referral, communication, and collaboration with pediatricians or medical specialists are important. A team approach ensures that complex cases receive comprehensive care, combining the expertise of multiple disciplines to optimize patient outcomes. My Peds Level 1 course will equip you with the tools to treat these issues effectively, without needing to refer all cases to specialists.
Myth #5: Pelvic Floor Dysfunction Can Be Treated With Kegels
It’s a widespread misbelief that Kegel exercises — contractions of the pelvic floor muscles — are the solution for most pelvic floor dysfunction. While Kegels can be helpful in some cases, they are not a universal remedy.
Fact: In children, pelvic floor dysfunction often involves hypertonic muscles that can’t relax properly, meaning Kegels might exacerbate the problem. Therapy for pediatric pelvic floor dysfunction typically involves a multiple-intervention approach, including techniques such as breathing, biofeedback, and behavioral interventions.
As a pediatric therapist, you’re already skilled in teaching children and helping them achieve milestones in their development. Pelvic floor therapy is an extension of your expertise, requiring you to learn new assessment and treatment techniques. In my Peds Level 1 course, I’ll guide you through the appropriate exercises, ensuring that your treatments are customized to meet each child’s unique needs.
Why Pediatric Therapists Should Learn Pelvic Floor Therapy
Incorporating pelvic floor therapy into your pediatric practice can add another dimension to your work, enabling you to treat children holistically and address issues that might otherwise go unresolved.
Here’s why you should consider expanding your practice with pediatric pelvic floor therapy:
- Increase your impact: Many children with pelvic floor dysfunction go undiagnosed, and their quality of life suffers. By learning to recognize and treat these issues, you can make a profound difference in their health and well-being.
- Broaden your scope of practice: Offering specialized care like pelvic floor therapy can set you apart and increase your referrals. Parents, pediatricians, and schools are always looking for experts who can address these complex issues.
- Enhance your professional development: Adding pelvic floor therapy to your skillset makes you a more versatile therapist, capable of treating a wider range of conditions and supporting your patients more comprehensively.
If you’re ready to take the next step in your professional journey, my Peds Level 1 course is designed specifically for pediatric physical and occupational therapists like you. This course will give you the foundational knowledge and practical tools you need to confidently identify and treat pelvic floor dysfunction in children.