As a pediatric pelvic floor therapist, you often work with families who feel like they’ve done everything “right” when it comes to toilet training—only to find themselves back at square one. Regression, resistance, and emotional outbursts are more common than you like to admit, and these signals often point to a deeper issue: a mismatch between developmental readiness and parental expectations.
In this blog post, I’ll share the case of a 3-year-old girl whose toilet training journey quickly turned into a source of frustration for both her and her mother. We originally discussed this case in my private membership Facebook group, KBB Village. You’ll get to explore what was really going on, how we reframed the problem, and how pediatric therapists like you can help parents recognize subtle signs of readiness, control, and sensory processing.
Toilet Readiness Case Presentation
Nora* was a 3-year-old whose mother reported frequent resistance during toilet time, particularly with urination. Nora wore underwear during the day (not pull-ups) and had regular bowel movements without signs of constipation or discomfort. She sat on the toilet without hesitation, suggesting that fear or anxiety around the toilet itself was not the issue. According to her mother, Nora had previously been toilet trained but had since regressed. She no longer reliably initiated or communicated when she needed to urinate.
The mother’s primary goal was for toileting to be a positive, stress-free experience. More specifically, she hoped her daughter would begin to independently recognize and communicate the need to go, without prompting or conflict.
Nora’s postural habits also stood out as clinically significant. Pelvic alignment and core control play a key role in developing bladder and bowel control. When postural stability is lacking, children may struggle to access sensory input from the pelvic floor or coordinate the muscles needed for complete voiding. I explore this connection, along with the developmental stages of bladder control and toilet training readiness, in a previous blog post.
With that in mind, let’s take a closer look at where Nora fell along the toilet training spectrum.

Toilet Training Readiness Framework
Let’s take a step back to assess where Nora truly was on the toilet training readiness continuum. These steps reflect a broader combination of physiologic, motor, cognitive, and emotional readiness.
Physiologic Readiness:
- The bladder can hold for 2 hours, child wakes from a nap dry
- The amount of urine is more substantial at one time
- Bowel movements are regular in the diaper
While Nora had regular bowel movements and could stay dry for long periods, so she had physiological readiness. But the following aspects indicate she was not quite toilet ready.
Gross Motor Skills:
- Child can physically don and doff clothing
- Child can get on and off the toilet independently
- The child has core control and can sit in a proper toileting posture
Nora could manage clothing and toilet transfers, but poor seated posture—chest leaning away from pelvis—indicated weak core alignment, which can interfere with pelvic floor activation and bladder awareness.
Cognitive Readiness:
- Is the child aware of urge?
- Do they feel uncomfortable in a dirty diaper and can express this?
- Can they follow simple steps?
- Can they express interoception in other areas of their life (i.e. hunger, thirst)?
Though Nora followed directions and sat on the toilet without resistance, she lacked interoceptive awareness and relied on external prompts rather than internal signals.
Social/Emotional Readiness:
- Is the child showing signs of wanting to be independent or like a sibling or peer?
- Do they desire praise from the caregiver?
- Are they ready to have a toileting schedule?
- Can they self regulate?
Nora’s resistance seemed rooted in a desire for autonomy, not fear or discomfort. She wanted control, but lacked the internal readiness to match, creating a disconnect that led to regression.
The reality was that Nora wasn’t initiating toilet use independently. She wasn’t reliably signaling before the need to go. And while she may have had some success earlier, it was based on prompted practice, not true skill mastery.
Toilet Training Regression Without Medical Cause
When a child is reported to have been previously “trained” and then regresses, it’s essential to ask what toilet training really looked like initially. In this case, Nora’s mother had been frequently prompting her daughter to sit on the toilet. There was little room for the child to feel her own urge to urinate or to communicate her needs proactively. Instead, the process became a cycle of external control.
This girl appeared trained, but the skills were parent-directed, not child-driven.
And this matters. When children don’t develop their own internal sense of timing and urgency, they may miss out on building interoception—the ability to detect internal body cues like bladder fullness. When toileting is externally managed, the child doesn’t get the chance to connect sensation with action.
In this case, Nora showed no signs of constipation, pain, or urinary tract dysfunction. She had normal bowel movements and could sit on the toilet comfortably. However, Nora consistently sat with her chest far away from her pelvis and was unable to sit upright with good core support. This kind of posture can impair the coordination of pelvic floor muscles and limit awareness of lower abdominal and pelvic sensation.

Are Toilet Tantrums Sensory Or Behavioral?
On the surface, this case could be framed as behavioral: a child who “refuses” or “throws tantrums” around toileting. But dig a little deeper, and you may see something much more nuanced: a child stuck in a power struggle without the internal awareness or developmental readiness to fully participate.
This is where your role becomes so important. As a pediatric pelvic floor therapist, you must look beyond behaviors to understand the underlying systems at play. Is this a sensory integration issue? Is it about emotional regulation? Is it biomechanical? Is the child simply not ready yet?
The parent in this case was kind, supportive, and clearly motivated to help her child succeed. But she was unintentionally taking over the process by prompting Nora frequently, guiding her to the toilet, and expecting her to respond based on timing, not sensation.
One of the first things to recommend is that the mother pause prompting altogether. Instead, introduce a check-in system for Nora. Have the mother ask her daughter:
“What does your bladder feel like right now?”
This small shift can give a child space to start reflecting on her own body, rather than responding to external cues.
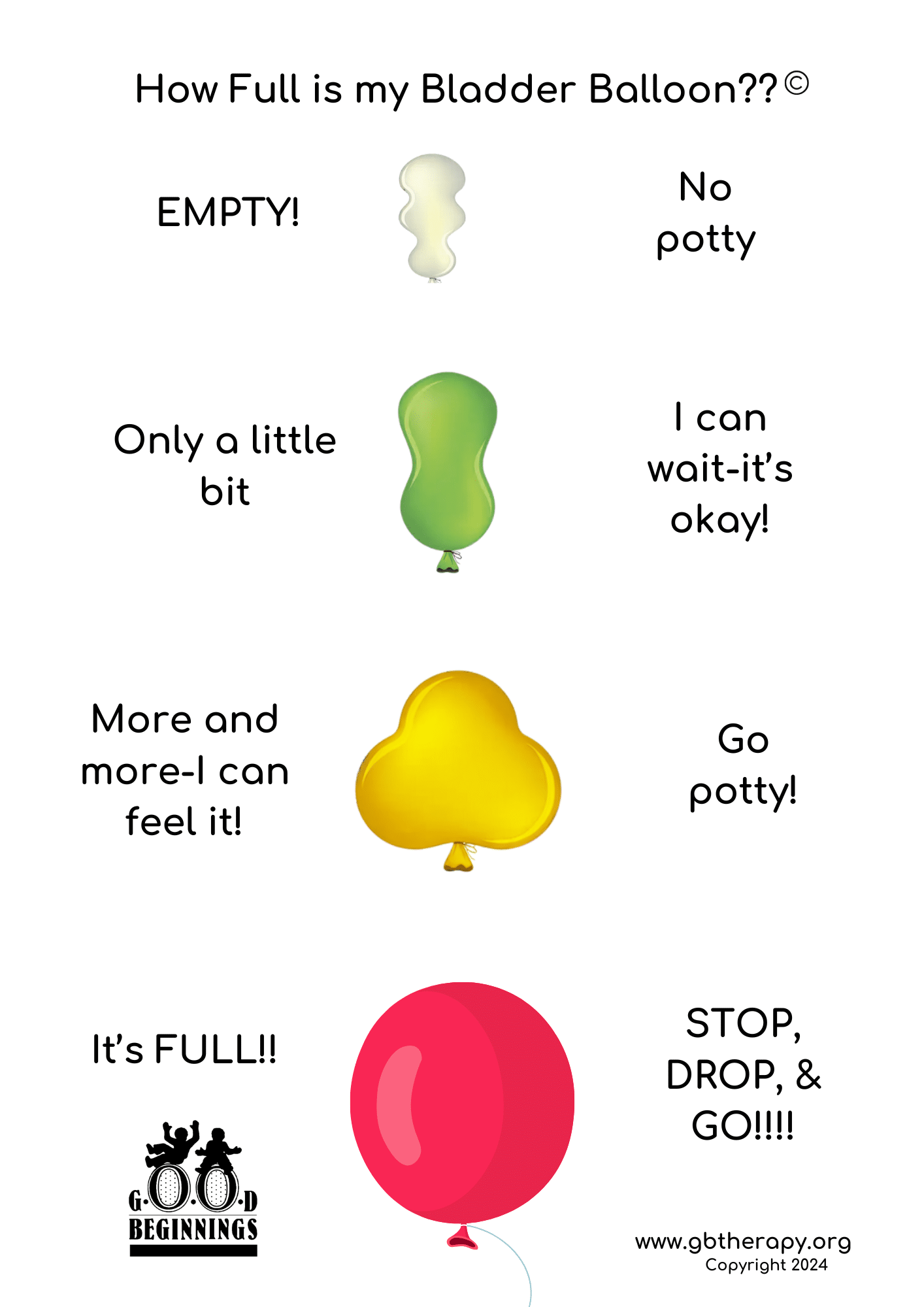
Introduce books and visual tools about interoception, using simplified body mapping activities and bladder rating scales like the Bladder Balloon Rating Scale (see below, courtesy of Amy O’Malley, PT, DPT, PCS at Good Beginnings Therapy). These tools allow a child to begin connecting internal sensations with external actions.
Key Takeaways For Therapists
This case serves as a powerful reminder that being “toilet trained” does not always mean a child is truly ready. Regression is not a sign of failure, but rather an opportunity to assess which systems may need additional support.
True readiness comes from internal awareness and self-initiation. Additionally, foundational elements like posture, core strength, and sensory integration play a significant role in how a child experiences and responds to bladder cues. As a therapist, you must also remember that parent education and emotional support are just as vital as your direct work with the child. Empowering families with tools, insight, and patience is key to long-term success.

Want To Learn More About Cases Like This?
This case is similar to many we explore in the Peds Level 1 online course, where we dig into:
- The neurophysiology of bladder and bowel readiness
- Behavioral and emotional components of toilet training
- Posture and movement as it relates to pelvic floor development
- Video demos and practical tools for evaluation and intervention
Whether you’re new to pediatric pelvic health or looking to deepen your clinical reasoning, this course is designed to give you the confidence to approach bowel and bladder cases comprehensively.
Join us for the next live Peds Level 1 – Treatment of Bowel and Bladder Disorders on August 24-25, 2025.
*patient’s name changed for privacy
