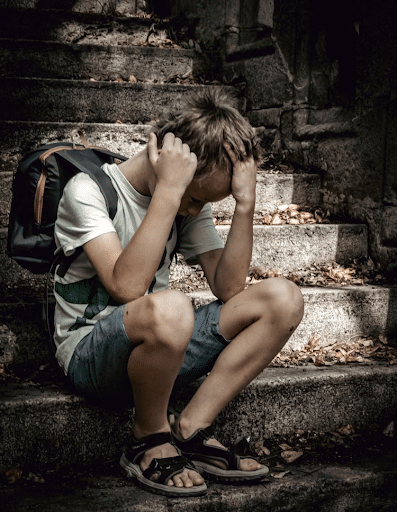
You know that sinking feeling when you realize a child in your care is hurting — not physically, but emotionally? You might notice they seem quieter than usual or less engaged in activities. Their parent mentions they’ve been “off” lately. You brush it off as a bad week… but what if it’s more than that?
As a pediatric pelvic floor therapist, you spend time with children and teens during some of their most vulnerable moments. You talk about bodies, private parts, and bathroom habits. These topics require trust and sensitivity. And because of that trust, sometimes kids will show you glimpses of their deeper pain.
That’s why having a strong foundation in recognizing emotional crises and youth suicide risk is so important. Knowing how to respond when something feels “off” is such an essential part of trauma-informed care.
Understanding Emotional Distress In Pediatric Therapy
Many young people are struggling with emotions they don’t know how to express. Between academic pressure, social media, and uncontrollable life stressors, today’s kids are carrying heavy loads. Add to that any history of trauma, anxiety, or family conflict, and it’s no surprise that so many kids are feeling hopeless.
As a therapist, you often see the ripple effects of that stress. Maybe a child’s pelvic pain flares up after a tough week at school. Maybe they regress in toileting after a fight at home. These may not be just physical reactions. They’re the body’s way of saying, “I’m not okay.”
When you are able to take a trauma-informed approach, you will recognize that pain and behavior changes can sometimes signal something much deeper than coordination or motor patterns. There’s no single “look” or behavior that defines a child in crisis.
Here are a few subtle signs that might raise a red flag. A child who:
- Suddenly seems disinterested in therapy, even if they used to love coming.
- Appears overly tired, distracted, or emotionally flat.
- Talks about feeling like a burden, or who makes negative comments about themselves.
You may also hear parents mentioning that their child is sleeping all the time, skipping meals, or losing interest in friends or sports.

These clues can easily blend into the background of pediatric life. After all, kids have ups and downs. But when your gut tells you something feels off, it’s worth paying attention.
How Pediatric Therapists Can Ask The Hard Questions And Take Action As It Relates To Suicide
This is where many therapists freeze. “What if I say the wrong thing?” “What if I make it worse?”
Here’s the truth: asking about suicide does not put the idea in someone’s head. In fact, asking can be one of the most powerful acts of care. It may give the child permission to speak what they may have been too scared to say out loud.
You don’t need to use complicated language. You can start with something like:
- “You seem a little different lately. How have things been going for you?”
- “Sometimes when kids feel really sad or stressed, they might have thoughts of wanting to hurt themselves. Has that ever happened for you?”
If they say yes, or even hesitate, take it seriously. Stay calm, stay with them, and let them know they’re not in trouble. You can say, “Thank you for trusting me with that. I want to make sure you’re safe. Let’s talk about who we can reach out to right now.”
If you ever suspect that a child may be at risk for self-harm or suicide, don’t wait. You don’t have to handle it alone, and you don’t have to be a mental health expert to help.

Building Connection And Safety In Pediatric Therapy Sessions
One of the most protective factors against suicide is connection — feeling seen, valued, and supported. As a pediatric therapist, you have an incredible opportunity to create that kind of connection in your sessions.
Every time you greet a child by name, celebrate their progress, or listen without judgment, you’re helping them feel like they matter. For some kids, that safe, consistent adult in the therapy room might be one of the few constants in their world.
That doesn’t mean you can fix everything, and you’re not supposed to. But your compassion can make a child feel less alone, and that’s often the first step toward healing.
Building Confidence In Trauma-Informed Pediatric Care
None of this is easy work, but it’s deeply important. When you learn how to recognize the signs of trauma, abuse and neglect, and suicide risk, you’re not just treating the pelvic floor. You’re treating the whole child.
If you want to feel more prepared and confident in navigating these difficult situations, my mini course, Pediatric Trauma-Informed Care, Child Abuse, and Youth Suicide, is designed just for you.
In the course, you’ll learn how to:
- Recognize the signs of emotional distress and suicidal ideation
- Ask the right questions in a calm, supportive way
- Navigate next steps if a child is in crisis
- Support your own emotional well-being as a provider

Working with kids who are struggling emotionally can take a toll. It’s okay to feel sad, worried, or even unsure of yourself. Make sure you’re also leaning on your peers, supervisors, or mental health support when you need it.
You can’t pour from an empty cup. Taking care of your emotional health helps you show up with calm, confidence, and compassion for the next child who walks through your door.
Every child deserves to feel safe. Every therapist deserves to feel equipped. Together, we can make that happen.
Enroll today in my online Pediatric Trauma-Informed Care, Child Abuse, and Youth Suicide mini-course today!
If you find the mini-course helpful, consider enrolling in my two other mini-courses:
AND
