You have undoubtedly witnessed the impact of unresolved issues like chronic constipation, bedwetting, or frequent urinary tract infections on a child’s life. Discomfort, anxiety, and even shame can become the norm for these kids.
Bowel and bladder challenges often fly under the radar in pediatric care, leaving many healthcare providers (including therapists like you) unprepared to tackle them effectively. Yet, identifying these symptoms as potential signs of pelvic floor dysfunction is essential to providing lasting relief and restoring a child’s confidence, comfort, and quality of life.

Pediatric pelvic floor therapy allows therapists to address the underlying causes rather than just managing symptoms. In this blog post, I delve into five pediatric conditions that could indicate pelvic floor dysfunction—and explain how addressing these can transform your approach to care.
Here are the conditions we will be looking at:
- Chronic Constipation
- Urinary Tract Infections
- Delayed Potty Training
- Enuresis
- Abdominal and Pelvic Pain
Chronic Constipation – Causes And Effects Of Pediatric Pelvic Floor Dysfunction
Chronic constipation may affect up to 30% of children worldwide, with many of these kids experiencing symptoms that persist for years. Chronic constipation is multifactorial, often influenced by diet, nutrition, behavioral patterns, and lifestyle habits. When the pelvic floor muscles are tight, weak, or uncoordinated, bowel movements become difficult, creating a cycle of strain, pain, and anxiety for the child.
This leads to the classic “chicken or egg” dilemma: does the child withhold stool because defecation is painful, or does it become painful due to withholding? Or, could an underlying anatomical issue be causing obstruction? Understanding these complexities is key to recognizing and effectively treating constipation.

Chronic constipation impacts children’s daily lives, leading to missed school days and social withdrawal driven by fear of accidents. By taking a holistic approach to treatment, you can offer families lasting solutions, alleviating the need for constant toilet-time struggles and temporary quick fixes.
With training in pediatric pelvic floor therapy, you gain the skills to assess muscle tone, movement patterns, and breathing habits that may contribute to constipation. Additionally, you will learn the important musculoskeletal sequelae that occurs when constipation is not managed. Through targeted exercises, biofeedback, and manual therapy techniques, you can help retrain these muscles, supporting children in achieving healthy, normal bowel function.
The Role Of Pelvic Floor Dysfunction In Urinary Tract Infections In Children
Urinary tract infections (UTIs) in children are sometimes dismissed as hygiene-related or due to bladder immaturity. However, pelvic floor dysfunction plays a significant role in many cases, especially when these infections are recurrent. When the pelvic floor muscles are uncoordinated or have high tone, this prevents complete bladder emptying, leading to urinary retention and increasing the likelihood of bacterial growth.
Children with recurrent UTIs may show hesitation in using the bathroom, complain of burning or pain during urination, or exhibit fear related to toilet routines. These signs may go unnoticed or are attributed to behavioral issues, but they may be early indicators of pelvic floor dysfunction.

Taking a comprehensive approach to the pelvic floor’s role in UTIs provides more effective, lasting solutions. By understanding how to evaluate and improve pelvic muscle coordination, you can help children achieve more effective bladder control, reduce infection rates, and alleviate bathroom-related anxiety.
You can use techniques taught in my online course including bladder training exercises, muscle relaxation methods, and behavioral strategies to support children in building healthier voiding habits. With these tools, you can play a crucial role in reducing UTI recurrences and helping children regain confidence and comfort with bathroom routines.
Delayed Potty Training As An Indicator Of Pelvic Floor Dysfunction
Children typically gain bladder control by age four, but the complex act of using the toilet requires both physiological and cognitive readiness. For kids experiencing delays in potty training, it is crucial to ensure that both the nervous and urinary systems are functioning properly.
As a therapist, your assessment can help identify the root cause in kids’ delayed potty training. Poor coordination of the pelvic floor muscles and bladder can hinder toilet training, leading to frustration for both children and their parents.
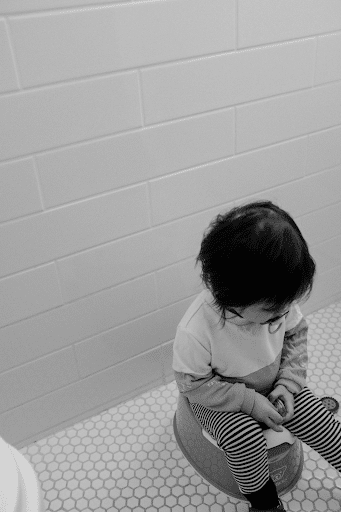
Delays in potty training can also cause embarrassment and anxiety, impacting a child’s confidence and social development. Some children may even develop avoidance behaviors, refusing to use the toilet due to fear or discomfort.
Understanding the connection between pelvic floor function and potty training will enable you to help families prepare with both physical and emotional readiness. Equip yourself with the tools to assess toilet readiness and support children experiencing delays in potty training, thereby creating a nurturing environment for this crucial developmental milestone.
Bedwetting (Nocturnal Enuresis) And Its Connection to Pelvic Floor Dysfunction
While bedwetting is commonly viewed as a normal developmental phase, it is a multifactorial condition often linked to pelvic floor dysfunction. For children with poor muscle coordination, bedwetting can result from hypertonic or weakened pelvic muscles that struggle to maintain control during sleep. These muscle imbalances can hinder the child’s ability to respond effectively to their body’s signals.
Interoception—the awareness of internal bodily sensations—plays a critical role in recognizing and managing bladder urges. Children with abnormal interoceptive skills may struggle to sense when their bladder is full or may have difficulty interpreting these signals, leading to challenges in controlling their urges. This lack of awareness can contribute to incomplete emptying before bed and subsequent involuntary bedwetting.

Strengthening and improving coordination of pelvic floor muscles through targeted exercises and behavioral techniques can help children better sense and control bladder urges and achieve complete bladder emptying.
The impact of enuresis extends beyond physical challenges; it can also lead to feelings of shame and social withdrawal as children grow older. When you can address enuresis in your practice, you will help alleviate these emotional burdens and rebuild the child’s confidence. Learn effective strategies to support children in achieving dry nights!
How Pelvic Floor Dysfunction Contributes To Abdominal And Pelvic Pain
Pediatric abdominal and pelvic pain can be challenging to diagnose, especially when medical tests reveal no clear cause. In many cases, the pain can stem from pelvic floor dysfunction, with hypertonic or uncoordinated muscles leading to discomfort during activities or prolonged sitting. Constipation is a common source of pain, as retained stool can lead to discomfort, while straining during bowel movements may exacerbate pelvic pain.
Children with abdominal or pelvic pelvic pain may avoid certain physical activities, complain about pain when sitting, or experience flare-ups after specific movements. If not addressed, this pain can limit their participation in school and extracurricular activities.
When you are trained to identify patterns of pelvic pain and assess pelvic floor function, you can often uncover the underlying cause and provide meaningful relief for children experiencing chronic discomfort. Learn how to help children return pain-free to the activities they love!

Many common pediatric symptoms might seem unrelated to pelvic health but can often signal underlying pelvic floor dysfunction. As a pediatric therapist, recognizing these connections enables you to offer more effective treatment solutions for children facing complex issues.
Are you ready to take the next step in expanding your expertise and improving pediatric patient outcomes? Join my Peds Level 1 pelvic floor therapy course to gain tools and techniques that will transform your practice.
