As a pediatric pelvic floor therapist, you sometimes see parents brushing off their children’s potty issues. Parents usually expect to have urinary challenges in the early years. More than not, those difficulties resolve as children develop.
But when children’s urinary symptoms persist, this should raise concern from parents and therapists regarding the possibility of vesicoureteral reflux.
Vesicoureteral reflux is even known as a silent condition, as it can go unnoticed until permanent damage is done. This is the most common urologic finding in children, causing renal damage in an estimated 21.8% of infants.
Early kidney damage can have life-long health consequences. Even though it’s beyond your scope as a therapist to diagnose this, understanding its etiology and the management of urinary voiding will help you when treating children with this condition.

What Is Vesicoureteral Reflux?
Vesicoureteral reflux (VUR) is the condition of retrograde passage of urine from the bladder into the upper urinary tract from the ureters into the kidneys.
The severity of the condition depends on how far up urine refluxes into the ureters and/or kidneys. Being familiar with the grades is important because the severity affects the likelihood of spontaneous resolution and necessary interventions.
There are 5 grades of VUR:
- Grade 1: urine refluxes part way up the ureter
- Grade 2: urine backs up all the way to the ureter
- Grade 3: urine backs up all the way to the ureter with dilatation of the ureter and renal calyces
- Grade 4: urine backs up all the way to the ureter with marked dilatation of the ureter and calyces
- Grade 5: massive reflux of urine with marked tortuosity and severe dilatation of ureter and calyces
Reflux into the kidneys can cause damage via inflammatory reactions with infected urine, causing scarring and fibrosis. Sterile urine can also cause damage via the backup of pressure.
There are multiple potential causes of urine backup in children. Let’s take a look at the primary and secondary causes of pediatric VUR.

Causes Of Primary Vesicoureteral Reflux
In a healthy urinary tract, urine reflux is normally prevented during contraction of the bladder. When the bladder contracts, it fully compresses the intravesical ureter, which is a segment of the ureter within the bladder wall. This muscular compression creates a seal at the ureterovesical junction, where the intravesical ureter lies, and prevents backflow up into the ureter.
Primary VUR is most commonly due to incompetent or inadequate closure of the ureterovesical junction, which allows urine to be pushed back up into the ureter. Failure of this anti-reflux mechanism is often due to a shortened intravesical ureter. The shortened length prevents the ureter from sitting fully embedded into the bladder, minimizing the ability of force closure at the ureterovesical junction.
The length of the ureter may be genetic, but it can develop into a better position with age and growth, as the ureter grows deeper into the bladder. The literature shows an 80% spontaneous resolution of primary VUR in grades I and II by age 5.
The likelihood of spontaneous resolution in children decreases with greater severity and laterality. Bilateral VUR is less likely to resolve than unilateral.
Now that you understand the mechanism of primary VUR, let’s further consider secondary causes.
Causes Of Secondary Vesicoureteral Reflux
Secondary VUR can be due to abnormally high pressure in the bladder that fails to close the ureterovesical junction during bladder contraction. This could be a result of hypertonic pelvic floor muscles. Increased pressure even in the absence of an anatomical problem can cause urine reflux.
Anatomical abnormalities which may also result in reflux include:
- Anatomical obstruction, such as posterior urethral valves in males
- Functional bladder obstruction
- Dysfunctional voiding
- Neurogenic bladder
As a pediatric pelvic floor therapist, understanding the cause of your patient’s reflux will help you in educating parents on the importance of healthy bladder and bowel habits. Let’s dive into the signs and symptoms you may see functionally.

Clinical Presentation And Early Diagnosis Of Vesicoureteral Reflux In Children
When diagnosed with VUR, establishing a voiding schedule for children is extremely important to empty the bladder fully and prevent excess urine reflux. Children with VUR may develop dysfunctional voiding patterns, especially if urinating is painful.
This causes increased urinary retention, which can lead to urinary tract infections (UTIs). Kids with VUR have higher rates of UTIs. In these cases, it’s standard to prophylactically treat with antibiotics, address constipation, and incorporate standard urotherapy.
With chronic UTIs and urinary retention, the bladder wall thickness increases.
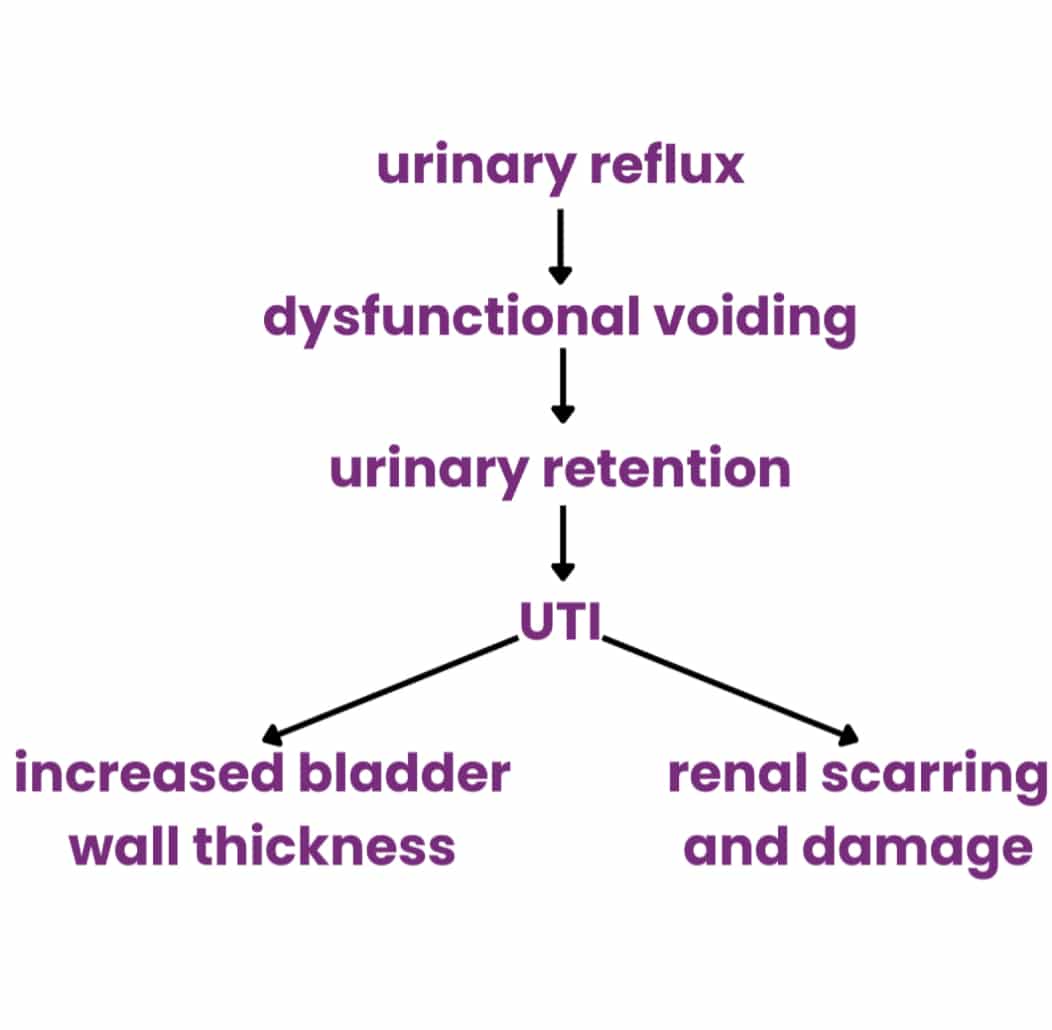
VUR can be detected early in utero with a prenatal ultrasound or at the first sign of a UTI. Febrile UTIs in infancy and early childhood are extremely concerning, as they can cause irreversible renal scarring. The early diagnosis of UTIs can help prevent the occurrence and severity of renal scarring.
Remember, our top priority is to prevent kidney damage in these kids!

Medical Management Of Vesicoureteral Reflux
Medical management in pediatrics depends on the severity of reflux and whether congenital abnormalities exist. The goal is to prevent UTIs and kidney damage while the child’s growth and development occur. Ideally, we will see spontaneous resolution of VUR as the child matures, but surgical intervention may be necessary.
Prophylactic antibiotics can prevent scarring by limiting infection and subsequent inflammatory reactions in the kidneys. This is often prescribed continuously for kids until they outgrow the reflux or until they are strong enough to undergo surgery.
Kids with VUR absolutely need to be seen for pelvic floor therapy preoperatively for bladder retraining, as well as post-operatively to promote and/or restore normal pelvic floor function. These children typically present with high resting tone, as opposed to the more common low tone you will see in your pediatric therapy practice. This high tone needs to be addressed by an expert to avoid long term issues and prevent recurrence of bladder (and other) issues down the road.
Bladder training is the cornerstone of medical management for pediatric vesicoureteral reflux. Options for surgical management exist on a case-by-case basis.

Ideally, your patients will not need surgical interventions. Your goal as a therapist is to maximize your kids’ safety and function before surgery and hopefully to avoid surgical intervention completely. Parent and patient compliance with therapy is paramount!
You don’t want to make parents fearful, but you must be confident in educating them about the significance of their child’s urotherapy program and the consequences if this diagnosis is left untreated.
Remember, the implications of kidney damage can last a lifetime! In addition to renal scarring, permanent damage can also include renal hypertension and chronic end-stage kidney disease. Let’s help protect these children by staying vigilant!
As you can see, there are few treatment options for VUR, and pediatric pelvic floor therapy is a huge component of treatment. These children and families need experts in their corner to assist them along this journey. Without a therapist trained in how to treat and support VUR, children will undergo unnecessary procedures every day.
Learn how to manage VUR today so no more children have to undergo medical management without a truly complete medical team (that includes you!) In my Peds Level 1 course you will learn exactly how to identify and treat VUR, with in depth instruction on the various presentations so you understand how to position yourself best on your next patients’ care team. Click to learn more about Peds Level 1 – Treatment of Bowel and Bladder Disorders: Evaluation and Treatment of Dysfunctional Voiding, Bedwetting, and Constipation.
Look forward to seeing you there!
Reference:
Vesicoureteral Reflux
