
What if I told you there was a missing link in the treatment of pediatric bowel and bladder conditions? As a healthcare provider working with pediatric patients, you know how common bowel and bladder issues, such as constipation and incontinence, have become in this population, and you’ve got plenty of tools in your treatment arsenal already, so what are you missing?
The answer may lie in a fairly recently discovered body system. We’re all familiar with other body systems, such as the nervous system, the urinary system, and the digestive system, which all play their own roles in the function of pediatric bowel and bladder conditions. But what is this other system? And what if I told you it kind of governs all the other systems?
This newfound “governor” of sorts is called the interoceptive system. In this blog, we will explore what interoception is, how it affects children with bowel and bladder dysfunction, the consequences of impaired interoception, and we’ll summarize some ideas on how you can start helping your pediatric bowel and bladder patients as soon as tomorrow.
What is Interoception and How Does the Interoceptive System (That You’ve Never Heard of) Work?
Interoception is the sense that gives us awareness of the internal sensations in our bodies, such as hunger, thirst, and fullness for example. It also plays a crucial role in our body’s ability to regulate functions such as breathing, heart rate, and bowel and bladder control. In children, interoception can be impaired due to various reasons such as developmental delays, neurodevelopmental conditions, history of trauma, and sensory processing disorders.
All of us have internal sensations within our bodies, and the different sensations are registered by receptors, located, well…everywhere. There are sensory receptors in your heart, lungs, stomach, bladder, and even the whites of your eyes. The job of these receptors is to continuously gather information about the specific condition or status of each body part or organ it’s associated with.
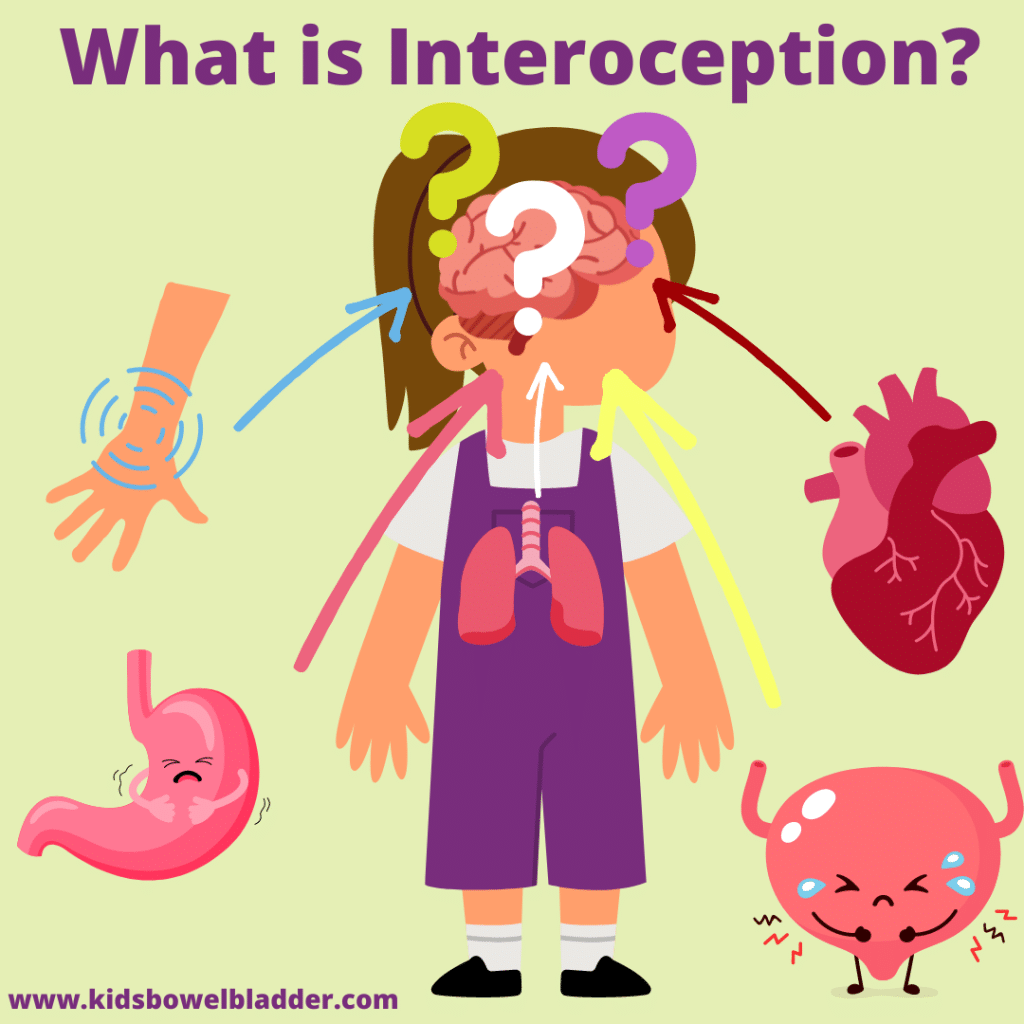
The information gathered from all around the body is sent to the brain, and the brain uses the information to regulate the body. The brain is always taking in information, which includes that of the interoceptive system, and making changes accordingly in order to maintain homeostasis.
This system starts to learn how different situations make our body feel over time, and “remembers” these feelings and sensations as a means of becoming more efficient. What this means is that the interoceptive system is actually predictive.
Consider this a good thing, because your body can quickly respond to something that’s the same over and over again (like sensing a full bladder, creating an urge to empty your bladder, causing you to go to the bathroom). The predictive nature of the interoceptive system can be unhelpful at other times.
For example, your 8-year-old patient, Sophie, can feel the sensation in her bottom that means her rectum is full. However, she’s not aware this means she should go to the bathroom. She regularly ignores the sensation of a full rectum.
Her interoceptive system learned that those signals to the brain would not result in Sophie being urged to empty her bowels, so to conserve energy, her receptors stopped signaling. Thus begins the vicious cycle of chronic constipation.
Does Interoception Have the Biggest Impact on Children with Bowel and Bladder Conditions?

Thankfully, we are learning more every day about different ways in which we can update the interoceptive system to work with the body, not against it. Interoception is experienced a little bit differently for every person.
While one child may say it feels like “pressure” when they have to use the bathroom, another may say it feels like “heaviness”.
As you can imagine, this can make it more challenging to manage pediatric bowel and bladder conditions. Considering how great of an impact these conditions have on childrens’ quality of life, we need to ensure we’re doing everything possible to assist them in navigating their own interoception signals.
Children with impaired interoception may have difficulty recognizing when their bladder is full or when it is time to have a bowel movement. They may also have completely lost access to certain sensory input as a protective mechanism. This can lead to urinary incontinence, constipation, and encopresis, causing embarrassment and discomfort, or worse — chronic conditions.
What are the Consequences of Treating a Child without Addressing Their Interoceptive System?
You may find that children with impaired interoception may also have difficulty regulating their emotions which can lead to anxiety and behavioral problems, among other issues. These children have trouble with awareness of their bodily sensations, and their emotions as well.
Treating a child for bowel or bladder dysfunction without addressing interoception is going to be more difficult. Many therapists are likely incorporating some interoception into treatment without even realizing it.

The key to managing pediatric bowel and bladder issues more effectively is understanding each child’s specific interoception signals and how the child describes them. And the best way to learn a child’s signals is to ask.
When you don’t know what a child means, or what interoceptive signals they’re referring to when they use certain words, how can you really help them understand their body?
Taking behavioral-only approaches to bowel and bladder issues is a losing battle, and can do more damage than good. In one of her blog articles, Toileting + Interoception, Dr. Kelly Mahler talks about the impact of focusing on external motivators in isolation. Without learning to notice and understand the signals coming from their bodies, children simply can’t improve their toileting skills, no matter how many rewards or stickers are given.
This is directly applicable to patients in your clinic. You wouldn’t treat constipation without addressing the pelvic floor, nor should you treat constipation without addressing the interoceptive system.
Once a child is able to tune into the internal sensations of their body, they’re much more likely to achieve success with urotherapy and other pelvic floor treatments.
How to Know if Interoception is an Issue for Your Bowel and Bladder Patients
Thankfully, there is hope for your patients! By helping your patients understand their own interoception and how it relates to their bowel and bladder dysfunction, you can better manage these conditions and improve each child’s quality of life.
Let’s use Wyatt as an example. Wyatt struggles with ADHD, constipation, and encopresis. He says he doesn’t notice when his underwear is soiled, even though his parents can smell it immediately.
If you jump right in to treating the pelvic floor, you’ve bypassed the opportunity to incorporate interoception work into your treatment plan. Think about why Wyatt doesn’t sense the stretched rectum, leaking stool, or soiled underwear.
When was the last time you asked a patient (or their parents) how they sense other parts of their body?
Try asking these questions as a starting point:

- Does Wyatt seem to know when he’s thirsty or hungry? Or do you have to remind him to eat or drink?
- Does Wyatt realize when he’s getting tired from playing/exercising? Or do you notice him often running until exhaustion?
- How does Wyatt react when he experiences something painful? Would you say his reactions are exaggerated or subpar?
Questions like these give you insight into the status of your patient’s interoception. Maybe they don’t notice their bowels, but if they don’t notice anything else either, the child’s problems are bigger than soiled underwear.
What Can You Do to Implement Interoception Into Your Treatment Recommendations Tomorrow?
The importance of interoception in the management of pediatric bowel and bladder dysfunction cannot be overstated. By understanding a child’s interoception, you can better identify the root cause of the child’s bowel and bladder issues and develop a personalized treatment plan.
This can lead to improved outcomes and a better quality of life for the child. With this knowledge, healthcare providers can better diagnose and treat these conditions, helping children overcome the challenges associated with impaired interoception.
When you’re looking to improve a child’s interoception, it’s important to meet them where they’re at. Start with very obvious interoception activities, such as sensing water and temperature on the hands.
When placing their hands in a bowl of cold water, what do they feel? Allow the child to describe their feelings and sensations so they’re unique to them. “Wet” and “cold” are pretty universal, and a great starting point for being able to explain interoception in a concrete way the child and parents can understand.
You can have your patient squeeze their fist tightly, and ask them how that feels compared to when the hand is relaxed. You can also allow them to get a little dirty, with some mud or dirt from outside. Inquire as to how the child interprets the different sensations. This is “Interoception: 101” for your patients.
Dr. Mahler typically recommends starting from the outermost parts and moving inward with interoception training. This training is essentially mindfulness, or noticing what’s happening with the body in the present moment. You may need to adapt the mindfulness activities to your patient so that they’re relevant to each individual and their current interoception abilities.
Moving Forward With Interoception and Treating Pediatric Bowel and Bladder Conditions

Today we learned about interoception, what it is, how it affects children with bowel and bladder conditions, and some things you can start doing to help your own patients with interoceptive challenges.
Dr. Mahler’s website has several free and paid resources if you’re interested in learning more about how you can implement interoception and this adaptive mindfulness into your practice.
The key to working with pediatric patients with impaired interoception is understanding how their specific interoception affects their ability to achieve or maintain bowel and bladder control. By understanding interoception and how it relates to pediatric bowel and bladder dysfunctions, you have a leg up on managing these conditions and improving your patients’ quality of life.
If you are a healthcare provider who treats pediatric patients and are interested in learning more about becoming a pediatric pelvic floor therapist, I invite you to sign up for my self-paced course, Peds Level 1 — Treatment of Bowel and Bladder Disorders: Evaluation and Treatment of Dysfunctional Voiding, Bedwetting, and Constipation. This course will give you a deeper understanding of pelvic health therapy specific to the pediatric population, teach you about the latest evidence-based practices for treating pediatric bowel and bladder dysfunction, and how to apply these practices to your patients.
Inside my self-paced course, you will also have the opportunity to ask questions within each module for clarification or a deeper understanding.
Once you’ve enrolled in one of my courses, you’re welcome to join the KBB Professional Village, my private clinical mentorship group where you can connect with other pediatric pelvic health providers who are dedicated to improving the lives of children with these conditions, ask questions about specific cases, and attend virtual Q&As twice a month.
As always, if you have any questions or would like to connect, please don’t hesitate to reach out.
