
If you’ve worked with children with enuresis for any length of time you’ve seen a child like Jackson.
Jackson comes bouncing out of his chair when you greet him in the lobby. He either runs or skips down the hallway. If you’re able to slow him down you notice he likes to walk on his toes.
He can be impulsive — darting towards pieces of exercise equipment in the therapy gym. If his mom has a chance to grab his hand, he’s pulling her down the hallway.
Once you enter the treatment space Jackson is full of excitement and energy. And before you can grab his attention he’s halfway up the rock climbing wall.
Jackson has attention-deficit hyperactivity disorder (ADHD). He’s eager to participate and loves all the fun activities you have him do during your treatment sessions. The downside — his body is so out of control he has a hard time participating in exercises to help stop his bladder leaks at night.
My last blog highlighted constipation as a primary cause of enuresis in children. This week, let’s explore the relationship between Neuropsychiatric disorders and enuresis.
The Link Between Neuropsychiatric Disorders Like ADHD, and Enuresis
To review, enuresis is a term used to describe children who leak urine while asleep no matter what the cause is. Before, the term nocturnal enuresis was used to describe bedwetting. It has been simplified to enuresis to describe bladder leaks at night.
There’s a strong relationship discussed within the literature between neuropsychiatric disorders and enuresis, specifically related to ADHD. Neuropsychiatric disorders are described as a comorbidity of enuresis and are related to dysfunction of the central nervous system.

Children with ADHD, like Jackson, and other neuropsychiatric disorders often have difficulty with:
- Arousal
- Sleep
- Circadian rhythms
All of these affect bladder function during the day and the night.
Children with autism spectrum disorder (ASD), another growing neuropsychiatric condition, often experience bladder and bowel dysfunction at higher rates than children without ASD.
Studies have shown children with ASD are 30% more likely to experience enuresis than other children. And 25% more likely to experience daytime urinary incontinence than other children.
A 2015 research article studying the relationship between ADHD and continence found positive outcomes in the treatment of enuresis when addressing a child’s inattention and impulsiveness.
The research also discusses more difficulty treating children with behavioral problems. It stresses the importance of early intervention for both non-pharmacological and pharmacological treatments.
You get it.
You’ve seen it.
You’ve had a patient like Jackson – the little boy or girl (although many neuropsychiatric conditions are more prevalent in boys) who can’t sit still.
Children like Jackson are not bad children, they simply don’t have control of their bodies. And like most children with ADHD, enuresis is not their only challenge.
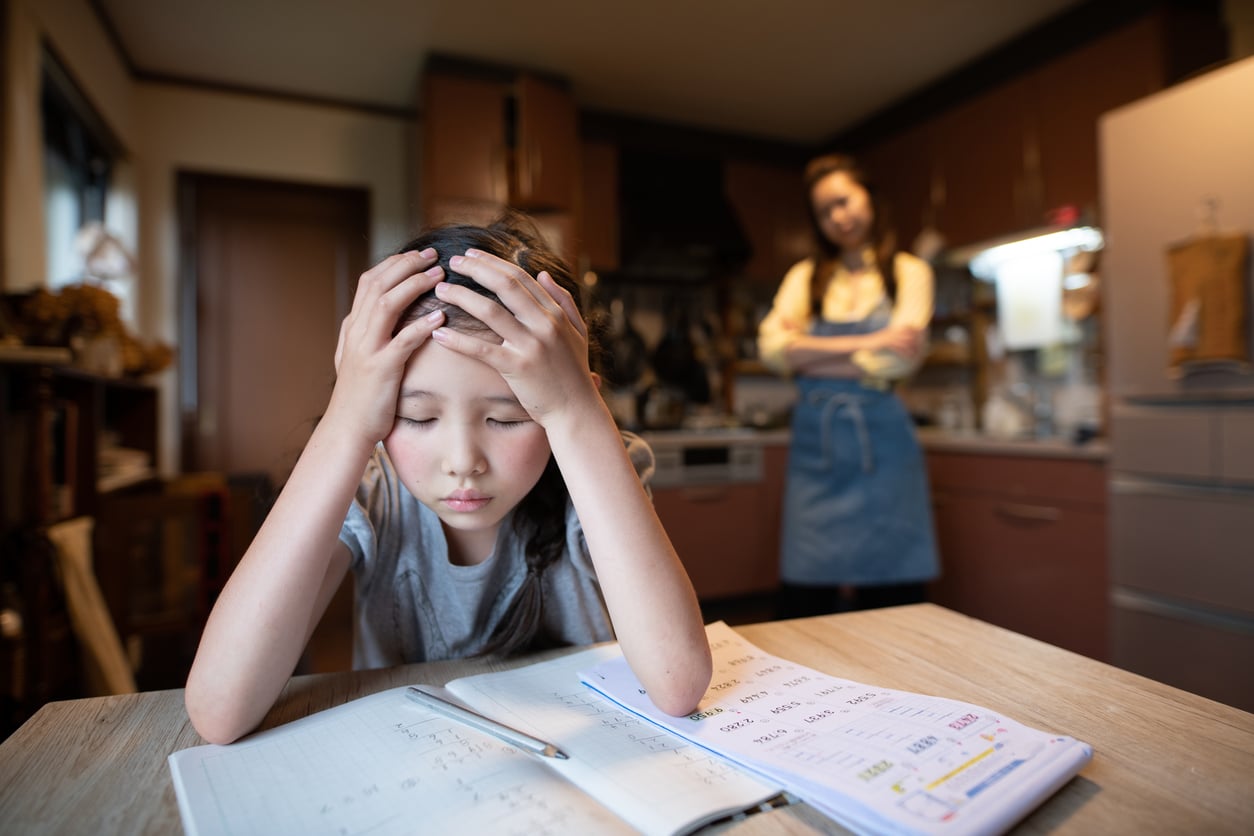
During the course of Jackson’s therapy, his mother has shared with you how he struggles in school. He has difficulty:
- Completing his assignments on time
- Staying in his seat
- Focusing on his work instead of his classmates
At home, he has hard time doing things like:
- Getting dressed in the morning
- Completing tasks greater than 1 step at a time
- Finding his belongings (as compared to other children his age)
His parents need to redirect him constantly to help him complete familiar daily activities.
So, how do you treat a child like Jackson who can’t sit still long enough to even say “enuresis”?
Treating Children with Enuresis and ADHD
Helping to regulate a child’s body with ADHD can be key in helping them achieve dry nights.
If your patient truly can’t sit still or attend to tasks long enough to participate in therapy for their bladder it may not be the right time for you to see them. This may be the perfect time to reach out to your friends in occupational therapy (OT).
I’ve often referred a child like Jackson to an occupational therapist and this can be key in helping a child with enuresis.
Sometimes a child may participate in occupational therapy for months before returning to my clinic to address their enuresis. Other times I’ve worked alongside OT while treating a child like Jackson.

Some simple tools can be helpful in improving their attention and participation in therapy. I like:
- Weighted blankets
- Changing the child’s body position
- Oral motor activities
OTs and PTs who are trained in sensory processing have a unique skill set and understanding of children with neuropsychiatric disorders including ADHD. Their primary goal is to provide sensory input into the child’s body to help calm their central nervous system.
A child with neuropsychiatric dysfunction is fighting a constant state of inner stress while trying to perform their daily activities. This ongoing struggle may include difficulty with:
- Visual attention
- Difficulty sitting still due to postural weakness
- Active primitive reflexes
- Shallow breathing patterns
- Muscle guarding and tightness
- Poor body awareness
Once a child is better able to regulate their nervous system, they’re able to:
- Tune into the internal signals of their body
- Recruit the pelvic floor musculature
- Withhold the urge to urinate while sleeping at night
Where to Learn More About Treating Children with Enuresis and ADHD
In my last blog I mentioned how hard it is to treat children with constipation and enuresis. The truth is, treating children with enuresis is hard no matter what.
This article has finally confirmed your suspicions about the relationship between enuresis, ADHD, and other neuropsychiatric disorders. But where do you go from here?
You may have other questions like:
- When should a child see an occupational therapist?
- What are some treatment ideas I could use right away to help my patients like Jackson?
- Are there common symptoms to look for in children who have ADHD and enuresis?
- And what about children with autism?
Unfortunately, there are no black-and-white answers. But having a greater understanding of how neuropsychiatric disorders like ADHD and autism relate to enuresis, you’ll be more effective in helping children become dry overnight.
My introductory course on kids bowel and bladder disorders helps you gain a greater understanding of how to treat children who wet the bed. You’ll learn about enuresis in addition to all of the other most common bowel and bladder diagnoses related to the pediatric pelvic floor patient. Become proficient in diagnosing, creating and carrying out treatment plans, and ultimately changing these childrens’ lives!

My courses are offered live using both in-person and online platforms, plus there is a self-paced option for therapists with a variety of learning styles.
Whether you’re just starting to treat children with bladder and bowel dysfunction or if you’re an experienced pediatric pelvic floor therapist, you’ll find a comprehensive course to take your skill set to the next level.
Learn how you can be more successful in the treatment of children with enuresis and ADHD by signing up today.
And don’t forget to sign up for my free ebooks on bedwetting and constipation to get you started.
Sources:
- Neuropsychological functioning related to specific characteristics of nocturnal enuresis
- Incontinence in children with autism spectrum disorder
- Incontinence in children with treated attention-deficit/hyperactivity disorder
- Behavioral problems in children with primary monosymptomatic nocturnal enuresis – ScienceDirect
