As a pediatric pelvic floor therapist, you often find yourself at the intersection of many disciplines—urology, gastroenterology, neurology, primary care, and more. One of the most critical conversations you may have to navigate is the communication with physicians regarding the Modified O’Regan Protocol (M.O.P.)—a structured enema-based program for treating refractory constipation and associated urinary incontinence.
While this protocol is increasingly accepted within certain specialties and by informed parents, many physicians remain unaware or resistant to its use. This can create friction, especially when a child is suffering and the family is desperate for answers.
In this blog post, I’ll unpack strategies to effectively and professionally communicate with physicians about M.O.P. I’ll explain why this protocol is often necessary after everything else has been tried, and how my Peds Level 1 course can prepare you to advocate confidently for your patients and their families.
When Nothing Works For Pediatric Constipation Or Incontinence: Why It’s Time To Consider The M.O.P. Protocol
One of the most common frustrations you probably hear from families is that they’ve already tried everything, and they’re not wrong. They have:
- Taken oral laxatives for months or even years and still presents with fecal leakage
- Had multiple bowel clean outs without resolution
- Followed through with behavioral strategies and reward charts.
- Made dietary changes, tackled sleep hygiene, and explored emotional regulation.
- Navigated co-existing challenges like anxiety or neurodivergence.
And yet, the child is still bedwetting, soiling, or withholding.
This is often when the M.O.P. program becomes necessary. Not necessarily as a first-line treatment, but as another approach with strong rationale—and for many families, the only one that finally works.
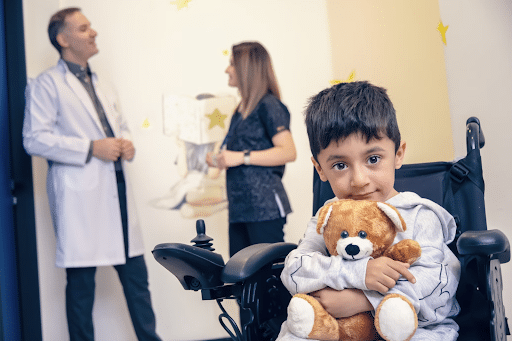
The Emotional Toll Of Incontinence And Why M.O.P. Matters
Consider a past case that I treated: Nate* was a bright and sensitive 3rd grader, who was emotionally devastated by continued bedwetting. His parents had already tried multiple cleanouts, sleep training, alarms, dry morning program and were working with me on pelvic floor biofeedback.
With minimal improvement in Nate’s bedwetting, they returned to the physician’s office, desperate. They saw the pediatric urology physician assistant, who told them to stop all laxatives and reassured them that Nate would “just grow out of it.” Worse, the PA told the parents that the “dry morning” approach was ruining their son’s sleep, with no evidence to back up his claim.

And because the guidance came from a physician’s office, the parents believed it.
“I think we’re just going to see a counselor now,” the mother later said.
These kinds of scenarios are heartbreaking, not only because they dismiss the complex interplay of bowel and bladder dysfunction, but because they leave the child and family without tools or hope.
Understanding Physician Resistance To Enema Use In Pediatric Constipation Treatment
When you bring up M.O.P. with families, you may hear this concern:
“My child’s doctor says enemas are traumatizing.”
Many physicians are simply unfamiliar with the research behind M.O.P. and how enemas, when used in a structured way, can be life-changing, not traumatizing.
What is more traumatizing for a child?
- A well-tolerated enema given at home with parent support
OR
- A daily life dominated by anxiety about leaking at school, hiding underwear, or getting teased by peers?
When children are asked, many would rather do an enema than suffer the uncertainty of incontinence in public.
Additionally, there’s a common belief among some physicians that constipation will improve without intervention. There is no evidence to support that statement and chronic withholding can lead to a megarectum, megacolon, rectal desensitization, and years of fecal and urinary issues. These are not kids who are “just behind.” These are kids with a significant functional disorder.

Research To Support Early And Aggressive Constipation Intervention
The longer a child’s constipation issue persists, the harder it becomes to treat—not just medically, but psychologically. Research shows that unresolved bowel dysfunction by age 6 can lead to long-term mental health impacts, including shame, anxiety, and social withdrawal.[1]
This is why I advocate for early and assertive interventions, including M.O.P., when conservative treatments have failed.
The International Children’s Continence Society (ICCS) recognizes functional constipation as a major driver of pediatric urinary dysfunction and outlines standard approaches, including enemas, when appropriate.[2]
When communicating with a resistant physician, one of the best tools you can use is the ICCS standardization document. You’re not recommending something fringe. You are referencing a standard of care recognized by pediatric urology, GI, and continence experts globally.
Strategies For Communicating With Physicians
So, how do you bridge the gap between what you know as pediatric pelvic floor therapist and what physicians believe?
1. Document the Journey
Before recommending M.O.P., be sure to carefully document all prior interventions. This shows you are not jumping to enemas as a first-line treatment. Use your notes to outline:
- Laxative regimens and results
- Behavioral programs attempted
- Dietary changes
- Any other clean-out protocols
- Pelvic floor therapy going well
This documentation allows you to show physicians that M.O.P. is being considered because everything else has failed, not because you’re bypassing standard care.
2. Share the ICCS Guidelines
Send physicians the ICCS guidelines and highlight the sections that discuss enema use. When backed by published clinical guidelines, your recommendation becomes less of a “PT/OT opinion” and instead a clinical standard.
3. Keep the Focus on the Child
Keep the communication child-centered. Phrases like:
- “We’ve seen a significant psychological impact from ongoing incontinence.”
- “The child is now withholding at school and avoiding social events.”
- “The impact goes beyond bowel movements. This affects self-esteem, emotional well-being, and quality of life.”
- Parents are frustrated with the Constipation Carousel
By grounding your advocacy in the child’s quality of life, you reduce the emotional charge and focus on shared goals.
4. Use Parent Advocates
Sometimes the most powerful advocate is a well-educated parent. When a family isn’t receiving adequate support or guidance from their current physician, especially after serious medical issues have been ruled out, they may benefit from seeking care elsewhere. For example, if a pediatric GI specialist is unwilling to support enema-based treatments, families often find more comprehensive support by returning to their pediatrician or vice versa.
Children with neurodivergence are frequently affected by chronic constipation, but that doesn’t mean they can’t improve with the right approach. While some specialists may dismiss their symptoms as purely “behavioral,” pediatricians and informed providers may be more open to considering the broader physiological and functional factors contributing to bowel dysfunction.
You could also recommend a consultation with Dr. Steve Hodges, the leading M.O.P. expert, who offers telehealth services. His team can guide the family through the full program.
This route empowers families while sidestepping the potential physician-therapist conflict.

Final Thoughts: Standing Up Without Burning Bridges
I know how delicate this dance can be. You want to advocate fiercely for your patient, but also respect the role of their physician. It’s a fine line.
But here’s the truth: you are often the one connecting the dots when no one else sees the whole picture. You are uniquely positioned to validate the child’s experience, empower the family, and gently challenge outdated narratives.
Always include the Primary Care Physician in your communications so they know you respect their opinion and want to work together. Once they understand you knowledge base on this topic the referral will follow!
With the right tools, support, and language—you can advocate for M.O.P. while keeping collaborative relationships intact.
That’s exactly why I’ve developed specialized courses and resources for pediatric pelvic health professionals—including the Kids Bowel & Bladder Professional Village and my online course, Peds Level 1: Treatment of Bowel and Bladder Disorders.
Inside the Village, you’ll find a supportive community committed to helping you grow your clinical expertise and confidence. We dive deep into essential topics like effective communication with physicians and evidence-based treatment strategies.
The Peds Level 1 course equips you with the exact tools, language, and research-backed knowledge you need to:
- Explain the rationale behind M.O.P. with clarity
- Identify the right time to transition from oral to enema protocols
- Support families with compassion
*patient’s name changed for privacy
References:
[1] Al-Beltagi, Mohammed; Saeed, Nermin; S Bediwy, Adel; Elbeltagi, Reem (2025). Breaking the cycle: psychological and social dimensions of pediatric functional gastrointestinal disorders. Royal College of Surgeons in Ireland. Journal contribution. https://hdl.handle.net/10779/rcsi.28806746.v1
[2] Definitions, indications and practice of urotherapy in children and adolescents: – A standardization document of the International Children’s Continence Society (ICCS)
Nieuwhof-Leppink, A.J. et al.
Journal of Pediatric Urology, Volume 17, Issue 2, 172 – 181
