
Interoception isn’t the only sensory system impacting bladder and bowel dysfunction in children.
A 2014 study of school-age children with urinary incontinence (UI) found 44% of children had difficulty with a sensory processing disorder.
Within this study, a large number of children showed poor registration of sensory input and auditory sensitivity. The children with low tactile sensitivity were five times more likely to have UI than other children.
The Pyramid of Learning shows three foundational systems needed to support a child. If a child cannot organize and process sensory input without the development of these foundational systems higher-level areas of development can’t be fully achieved.
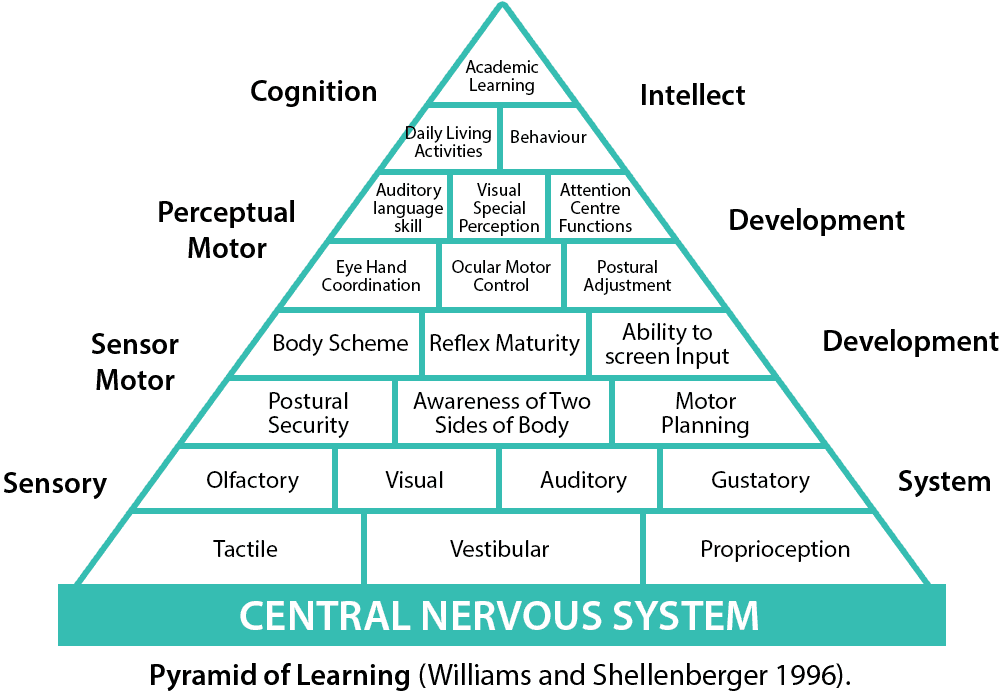
Understanding these three foundational sensory systems can help you be more effective in treating bladder and bowel dysfunction in children with a sensory processing disorder.
How Bladder and Bowel Dysfunction Is Related to Structures in the Brain
It’s no secret bladder and bowel function is related to structures found in and around the brain stem. These structures also play a vital role in one’s emotional regulation.
When treating children with a sensory processing disorder it is important to understand how emotional regulation can impact bladder and bowel dysfunction.
A small study comparing two groups of children identified microstructure abnormalities in children with primary monosymptomatic enuresis.
The researchers observed changes in the:
- Thalamus
- Medial frontal gyrus
- Anterior cingulate cortex
- Insula
All of these structures are involved in bladder control.
A delay in the development of these structures can contribute to bladder and bowel dysfunction in children.
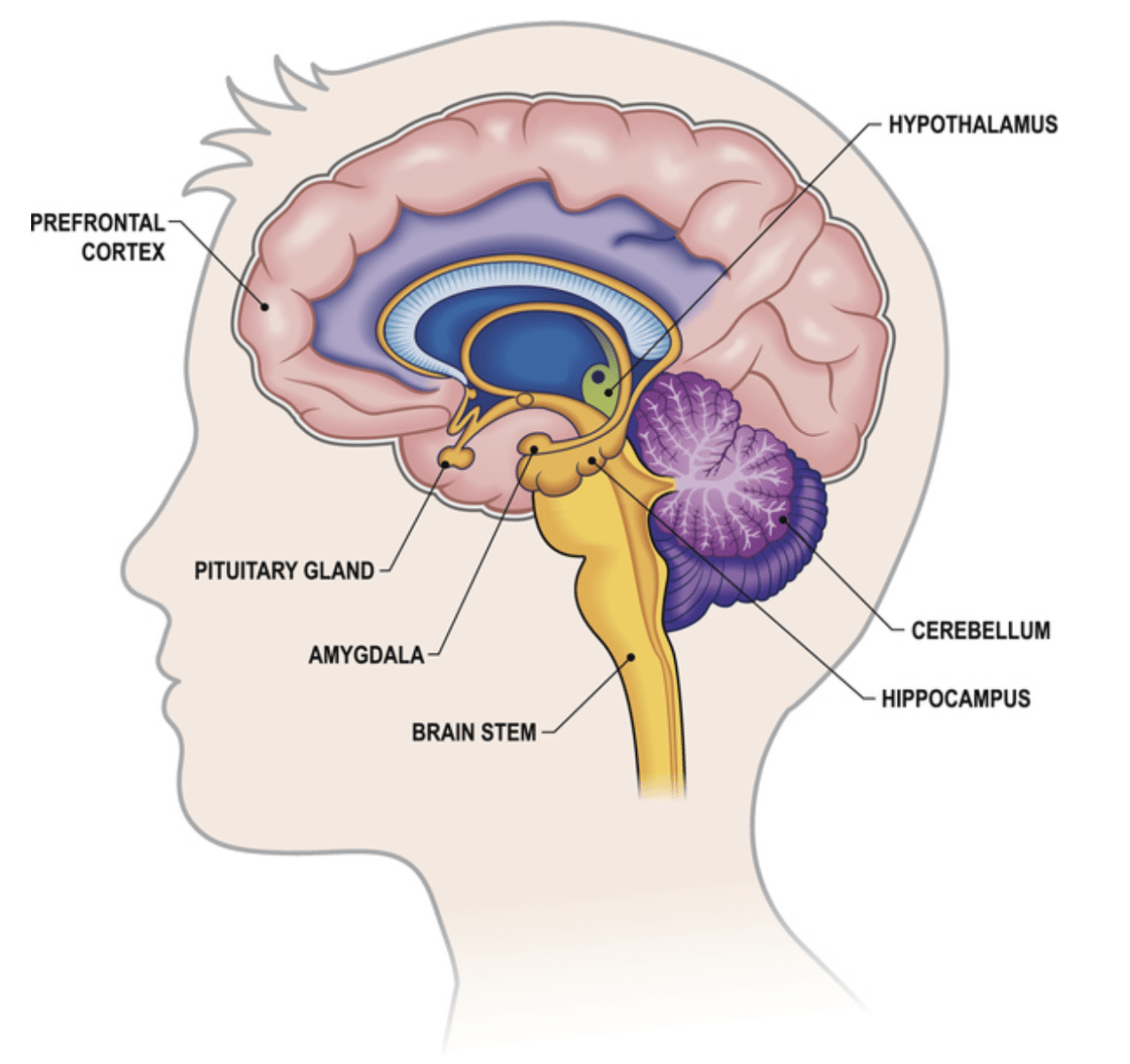
We also know there is a relationship between the limbic system, the emotional center of our brain, and our prefrontal cortex.
These systems are in constant contact with our bladder and our digestive system. It makes the decision of whether to eliminate or inhibit the urge.
When you become stressed or experience a “fight or flight” response the brain stem and surrounding structures including the limbic system become overloaded with sensory information. This can prevent your ability to interpret signals from the body to the brain.
This is why many of us experience urinary frequency before or during stressful events like public speaking.
For a school-age child an overstimulating classroom can raise their stress level to a point where they lose the connection between their body and their brain. They’re so overloaded with sensory information they can’t sense the urge to eliminate.
The Pyramid of Learning, teaches us which foundational sensory systems help us to understand and organize sensory information.
If we understand what our body is telling our brain we can take action.
If a child senses the urge to urinate they can contract their pelvic floor to stop their bladder from leaking until they can use the toilet.
Three Important Sensory Systems Affecting Bladder and Bowel Dysfunction in Children
Sensory integration describes how your nervous system understands and organizes sensory information. And how you respond to this information.
For a child who has a sensory processing disorder this ability to take in sensory information from our environment and appropriately respond to it can be a challenge.
The Pyramid of Learning is a map of how our vestibular, proprioceptive, and tactile systems are key in the development of higher-level skills.
Dysfunction in any one of these systems is often found in children with a sensory processing disorder. Not only can these systems disrupt a child’s ability to regulate their emotions, but can also play a role in bladder and bowel dysfunction.
- Vestibular Processing
Vestibular processing organizes sensory input from the movement of the body through space.
Many of us associate vestibular processing with balance. To help us maintain balance our body must send signals to the brain in response to how our body is moving. The fluid of our inner ear changes with our head position and helps send this information to the brain.
This is why it’s important to ask a child’s family if there is a history of ear infections or allergies. Chronic ear infections or allergies will increase the fluid in the ear and cause inflammation. This results in stiffness in the inner ear and impacts a child’s ability to process vestibular input.
Children who have difficulty with sensory processing may not only demonstrate difficulty with balance but may demonstrate “gravitational insecurity.”
Gravitational insecurity is when a child does not feel in control of their body in space. A child may be afraid to:
-
- Climb a ladder
- Sit on a swing
- Hang upside down

They may not like sitting on an adult-size toilet because they feel unsupported and are worried they will fall. Improving postural stability can help develop a child’s sensory processing, making them feel more secure.
The vestibular system also helps us to interpret what we hear.
Sometimes children with a sensory processing disorder demonstrate sensitivity to loud noises like:
-
- A vacuum cleaner
- A lawnmower
- A flushing toilet
- Automatic hand dryers
When they hear these sounds it can put their body into a “fight or flight” response. A child may no longer accurately interpret information within their environment.
If this has happened before, a child may have a PTSD-like response. They’ll be unable to eliminate in public spaces or in school because their stress level is too high and they can’t relax their body.
Can you see how a steady stream of mixed signals can result in bladder and bowel dysfunction in children?
2. Proprioceptive Processing
The proprioceptive system interprets sensory information from our joints and muscles in the body. The proprioceptive system relates to body awareness and how a child understands the amount of force needed to carry out a function.
Children with poor proprioceptive processing are often seen jumping and crashing into the wall, the floor, and other kids. They may use excessive force when coloring or writing. They’re unable to gauge the right amount of strength needed for a task.
Poor proprioceptive processing could lead to dysfunctional voiding if a child attempts to empty their bladder or have a bowel movement before relaxing their pelvic floor causing them to strain.
Using a sensory integration approach and incorporating proprioceptive input into your sessions can help calm a child’s nervous system. And help them tune into the internal signals of the body like the urge to eliminate or understand how to relax the pelvic floor when voiding.
3. Tactile processing
The tactile system helps you understand touch. This includes:
-
- Light touch
- Deep touch
- Vibration
Temperature
Pain
A child with poor tactile processing may not like the feeling of certain types of clothes, getting their hair cut, or may be a picky eater – adding another layer of difficulty when they’ll only eat processed food like chicken nuggets and french fries.
If a child is hyposensitive to tactile input they may not recognize the feeling of urine on their skin.
If they’re hypersensitive they may withhold the urge to have a bowel movement because:
-
- They don’t like the feeling of stool leaving their body
- It has been painful in the past
- They don’t like being wiped.

Some children who are hypersensitive may run and hide to have a bowel movement instead of using the toilet.
Some children are so hypersensitive to the feeling of an urge to have a bowel movement they’ll withhold stool and inhibit the urge. The body will respond by allowing the colon to stretch, withholding more stool, leading to a vicious cycle of constipation.
If any one of these systems is disrupted the skills we need to recognize the urge to eliminate and act upon that urge can affect a child’s ability to achieve continence.
Learn How the Kids Bowel and Bladder Professional Village Will Help
Understanding how our bodies process sensory information is foundational in human development.
Understanding how one system builds on top of another is crucial when treating children with bladder and bowel dysfunction who have a sensory processing disorder – as if treating children wasn’t challenging enough!
The KBB Professional Village is the perfect environment for sharing information on complex topics like sensory processing.
This ongoing monthly mentorship meets two times per month to discuss topics like sensory processing disorder and interoception. And other topics related to bladder and bowel dysfunction in children.
I invite experts to help us understand complex topics and influence our ability to effectively treat children with bladder and bowel dysfunction. Plus we review challenging cases to help guide you in your treatment.
In order to subscribe to this amazing group you need to first take my introductory course:
This comprehensive course has everything you need to get started.
Or if you’re an experienced pediatric pelvic floor therapist this course will provide you with:
- Up-to-date evidence-based research
- New treatment ideas
- Patient handouts
Peds Level 1 will help you grow your therapy toolbox when treating bladder and bowel dysfunction in children.
Stay tuned as I share what sensory processing red flags to look for in children with bladder and bowel dysfunction.
Sources:
- Sensory processing differences and urinary incontinence in school-aged children
- Changes in the Brain Microstructure of Children with Primary Monosymptomatic Nocturnal Enuresis: A Diffusion Tensor Imaging Study – PMC
- Peeing your pants: Why do people urinate when they’re scared?
- Sensory Integration – StatPearls – NCBI Bookshelf
