
I recently sat down with Dr. Steve Hodges, M.D. to discuss the impact of bowel and bladder disorders on children’s emotional well-being and overall quality of life. We also discussed the importance of a multidisciplinary approach to treating these disorders, the impact of early intervention, and resources for therapists and families.
Dr. Hodges is not only a urologist. He’s a professor at the University of Wake Forest, and a renowned expert in the field of treating enuresis and encopresis. His cornerstone work includes development of the Modified O’Regan Protocol for treating constipation and bedwetting, better known as the M.O.P. Book.
Dr. Hodges and I have worked closely together for years, blending our areas of expertise to continually improve outcomes for constipated children. Let’s dive into the interview.
Q: How can therapists/clinicians help parents and caregivers better understand the impact of bowel and bladder disorders on their child’s emotional well-being and overall quality of life?
A: “Enuresis and encopresis take a huge hit on kids’ self-esteem. Kids feel deep shame and can become very stressed. Accidents are not ‘normal,’ no matter how much society tries to normalize and downplay them. I try to tell parents: ‘common’ is not the same thing as ‘normal,’ and no one benefits from delaying treatment for enuresis or encopresis.”
I wholeheartedly agree with Dr. Hodges here. I even take his advice a step further and recommend against using the word “accident” with kids and families all together. “Accident” implies the child made a mistake, that there’s something inherently ‘wrong’ with them, which simply isn’t the case.
Working alongside the urologists, GI doctors, and pediatricians also treating your patients is the best way to tackle issues such as enuresis and encopresis. Although pediatric pelvic floor therapists are the last professionals to join a treatment team a lot of the time, that doesn’t mean we don’t have an important role. Educating your local multidisciplinary providers about what you do as a pediatric pelvic floor therapist is critical.
Q: Can you discuss the importance of a multidisciplinary approach to treating bowel and bladder disorders in children, and how therapists/clinicians can collaborate effectively with other healthcare providers?
A: “Many parents have told me that pelvic floor therapy was the ‘last piece’ or ‘missing link’ in treatment for a complete recovery from enuresis and encopresis. I believe pelvic floor therapists should make sure families understand that constipation is the root cause of enuresis and encopresis and that resolving the constipation is critical.
One specific treatment, biofeedback, helps kids understand that they are contracting muscles they thought were relaxing, and vice versa, and that really hits home with some kids. This is a specific treatment offered primarily by physical and occupational therapists.
At the same time, I think it’s important for therapists to promote bowel emptying. I’ve had many patients who, prior to seeing me, had undergone PT without an aggressive program to resolve their constipation. The rectum must be fully evacuated on a daily basis and have a chance to heal.”
I’m so glad Dr. Hodges brought this up. It’s one thing to be a pediatric pelvic floor therapist, having taken some coursework specific to the pediatric population. However, taking courses, and truly knowing how to treat the individual in front of you are two different things.
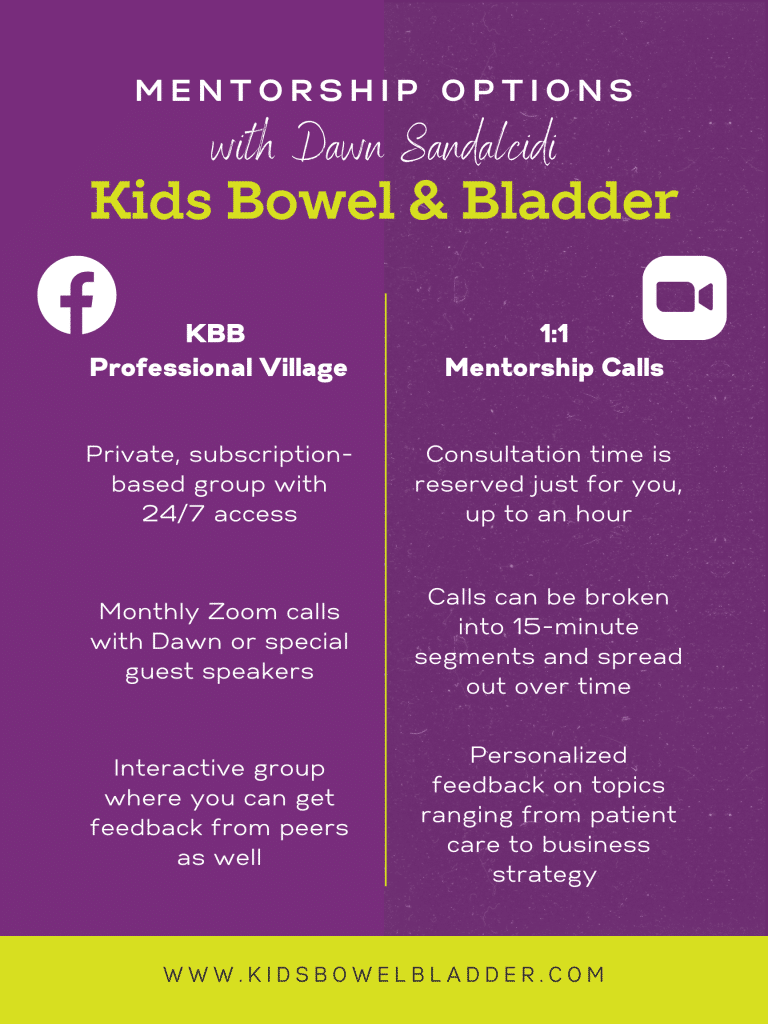
Children are not simply “small adults”. Bowel and bladder issues in the pediatrics are unique, and need to be treated as such. Sometimes, the best way to learn is by doing, which is why I do offer ongoing mentorship in a few different ways:
Q: Can you discuss the impact that early intervention can have on the long-term outcomes for children with bowel and bladder disorders, and how therapists/clinicians can play a role in advocating for early diagnosis and treatment?
A: “I believe all toilet-trained children who have persistent accidents, even if they are age 2 or 3, should be treated for the underlying constipation, and I believe that children who only have nocturnal enuresis should be treated at age 4.
Parents and physicians alike tend to brush off accidents, assuring families ‘Don’t worry, she’ll outgrow it.’ But I have a huge caseload of teens and tweens who were fed that line for years on end.
Left untreated, constipation often worsens and the tendency to delay pooping becomes more deeply ingrained. Treating a 4-year-old for enuresis is a lot easier than treating a 14-year-old or an 18-year-old.”
100% agree here! It’s certainly much easier to treat those children who are lucky enough to be referred to us quickly.
Treatment when started early is not only easier, but often lasts for a shorter amount of time as well.
Q: Can you recommend any resources or tools that therapists/clinicians can use to educate themselves and their patients about bowel and bladder disorders in children?
A: “I’ve recently updated and overhauled The M.O.P. Anthology: The Proven Way to STOP Bedwetting, Daytime Enuresis, Encopresis, and Chronic Constipation in Toddlers Through Teens. The brand-new 5th Edition includes detailed treatment regimens, the scientific backing for our approach, charts to track a child’s progress, and tons of other information to help families resolve these conditions more quickly and effectively.
The book emphasizes that chronic constipation is the root cause of enuresis and encopresis — that these are not psychological or behavioral conditions. Children should never be shamed or blamed for accidents.
My children’s books emphasize these points, too, with humor and compassion to help kids feel less alone. Bedwetting and Accidents Are Not Your Fault is for kids under 10. Emma and the E Club, our middle-grade novel, resonates with kids ages 8 to 12 (and sometimes younger). M.O.P. for Teens and Tweens will reassure middle school and high school students they’re doing nothing ‘wrong’ and their condition is totally fixable.”
A Special ‘Thank You’ to You, Dr. Hodges! I really appreciate you taking the time to chat about these important topics.
Therapists are learning about the world of treating pediatric bowel and bladder conditions daily. Having professionals like you supporting those taking this leap is important.
For any providers currently treating children, or pelvic floor patients — if you’re reading this and you’re interested in furthering your knowledge in the kids bowel and bladder field, check out my courses below to learn more!
